A normal Head, Eyes, Ears, Nose, and Throat (HEENT) examination is an essential part of a comprehensive physical examination. It allows healthcare providers to assess the overall health and functioning of the head and neck region, as well as detect any abnormalities or signs of disease.
During the examination, the healthcare provider will carefully inspect and palpate different areas of the head and neck, including the scalp, face, eyes, ears, nose, mouth, and throat. They will evaluate the patient’s physical appearance, skin condition, and the integrity of various structures in these areas.
The objective of documenting a normal HEENT exam is to record the absence of any significant findings or abnormalities. This documentation serves as a baseline for future reference and comparison, and helps healthcare providers monitor the patient’s overall health and detect any changes that might occur over time.
Key elements to include in the documentation of a normal HEENT exam may include observations such as clear and symmetrical visual acuity and visual fields, normal pupil size and reaction to light, intact extraocular movements, clear and equal hearing, absence of any nasal obstruction or discharge, normal oral and throat examination, and absence of any swelling or tenderness in the head and neck region.
Importance of HEENT Exam Documentation
In medical practice, a comprehensive examination of the head, eyes, ears, nose, and throat (HEENT) plays a critical role in assessing a patient’s overall health and detecting any potential abnormalities or conditions. Proper documentation of the HEENT exam is essential for several reasons.
- Accurate diagnosis and treatment: A thorough HEENT exam can reveal important information about a patient’s health status and provide vital clues for diagnosis and subsequent treatment. Documentation ensures that the findings are recorded accurately, enabling healthcare providers to make informed decisions and provide appropriate medical care.
- Track changes over time: Documenting the HEENT exam allows healthcare providers to track changes in a patient’s condition over time. By comparing previous exam results with current ones, doctors can identify any progression or regression of symptoms, helping them monitor the effectiveness of treatment plans and make necessary adjustments.
- Legal and medicolegal purposes: Accurate and detailed documentation of the HEENT exam is crucial for legal and medicolegal purposes. In case of any disputes or medical negligence claims, documented evidence can serve as a proof of the healthcare provider’s actions, decisions, and assessments during the examination, ensuring transparency and accountability.
- Continuity of care: Documented HEENT exam findings facilitate smooth communication and collaboration among healthcare professionals involved in a patient’s care. When different providers have access to comprehensive documentation, they can make well-informed decisions and provide consistent care, ensuring continuity and improving the overall patient experience.
In conclusion, proper documentation of the HEENT exam is imperative in healthcare practice. It enables accurate diagnosis and treatment, aids in tracking changes over time, supports legal and medicolegal purposes, and ensures continuity of care. By documenting the findings of the HEENT exam, healthcare providers can provide quality healthcare services and improve patient outcomes.
Head
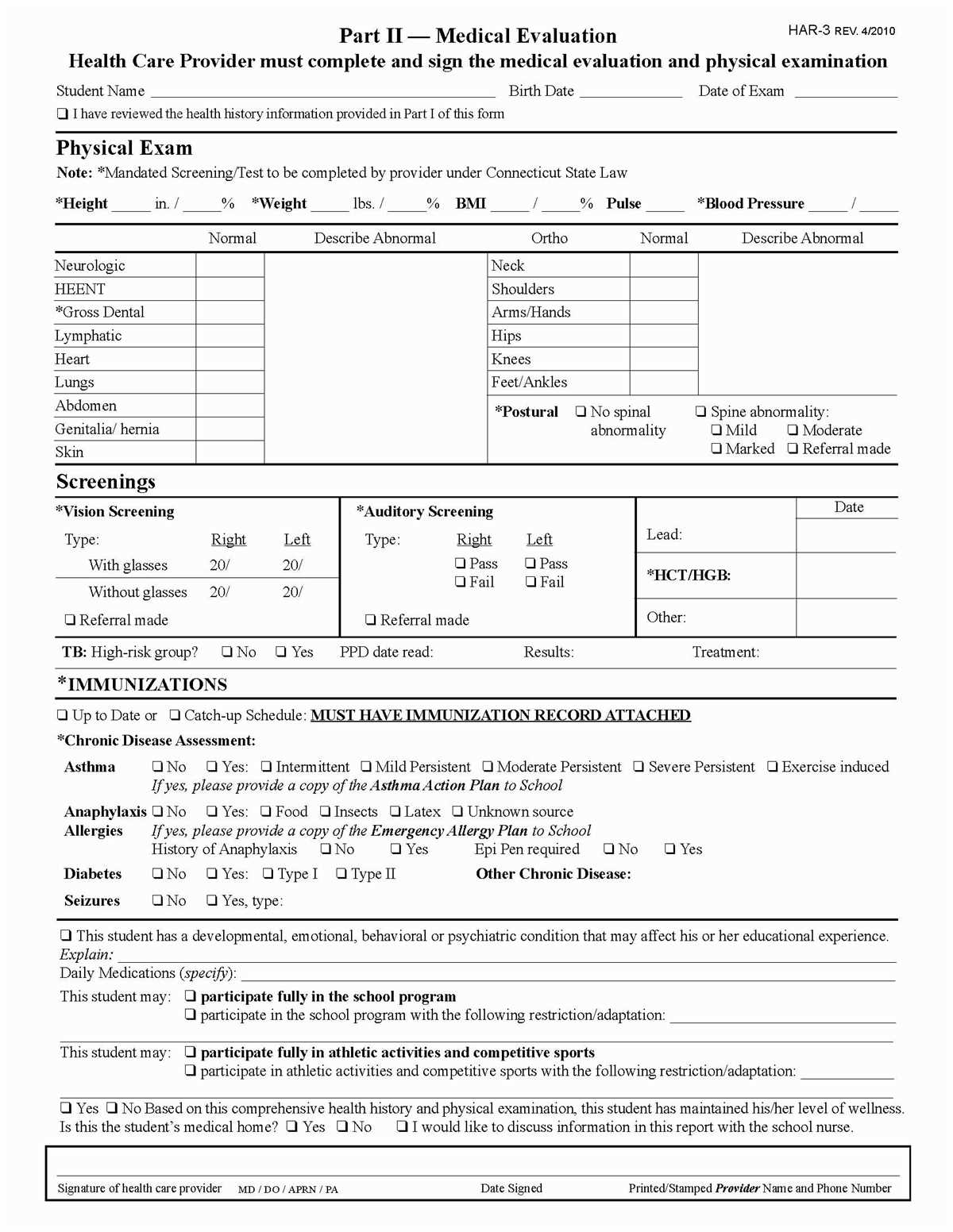
The head is an important part of the HEENT exam, as it provides a visual assessment of the structure and function of the cranial and facial regions. The examiner should inspect the head for any abnormalities, asymmetry, or signs of trauma.
During the examination, the examiner should assess the size and shape of the head, noting any deformities or irregularities. Additionally, the examiner should palpate the scalp for tenderness, masses, or abnormalities. The presence of any lumps, bumps, or lesions should be documented and further evaluated if necessary.
- Inspect the shape and symmetry of the head
- Palpate the scalp for tenderness or abnormalities
- Note any lumps, bumps, or lesions on the scalp
- Assess for signs of trauma or deformities
- Check for the presence of facial asymmetry or abnormal movement
In addition to the physical examination, the examiner should also assess the patient’s facial expressions and any abnormalities in facial movements. The presence of drooping, weakness, or asymmetry could indicate underlying neurological or muscular issues and should be documented.
Overall, a thorough examination of the head is important in the HEENT assessment to identify any potential abnormalities or concerns that may require further evaluation or intervention. Proper documentation of findings is essential for accurate diagnosis and treatment.
Examining the Scalp
When performing a HEENT (Head, Eyes, Ears, Nose, Throat) examination, it is important to thoroughly evaluate the scalp for any abnormalities. The scalp is comprised of the skin, hair follicles, and underlying connective tissue, and can provide valuable information about a patient’s overall health.
During the examination, the healthcare provider should first inspect the scalp visually, looking for any signs of inflammation, lesions, or discoloration. An assessment should be made regarding the patient’s hair distribution, thickness, and texture. Any areas of hair loss or thinning should be noted and documented.
Next, the provider should palpate the scalp, gently pressing on different areas to check for tenderness or irregularities. This can help identify any abnormalities such as lumps, bumps, or cysts that may be present beneath the surface. If any masses or abnormalities are detected, their size, location, and associated symptoms should be documented.
- Hair quality: Document the distribution, thickness, texture, and presence of any thinning or bald patches.
- Scalp lesions: Note any inflammation, rashes, lesions, or discoloration found on the scalp.
- Palpation findings: Record any tenderness, irregularities, masses, or cysts felt during palpation.
Overall, a thorough examination of the scalp is an essential component of the HEENT assessment, as it can provide valuable insight into a patient’s dermatological and overall health status.
Evaluating the skull
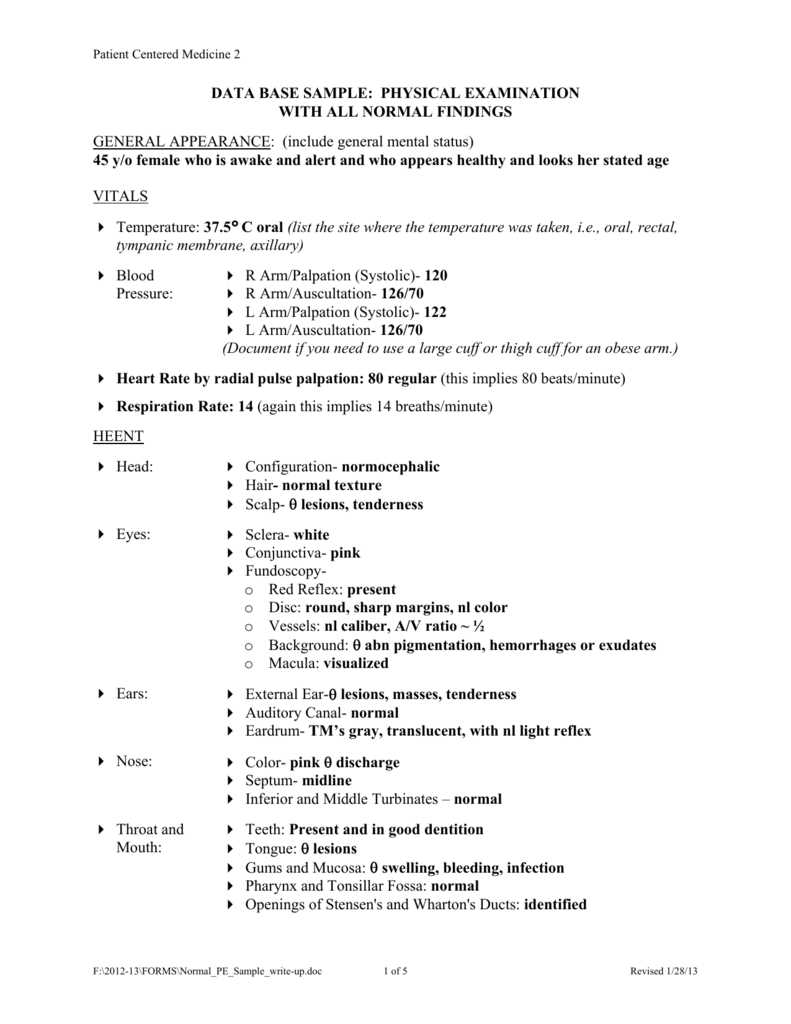
The evaluation of the skull is an important component of the HEENT (head, eyes, ears, nose, and throat) exam. It provides valuable information about the overall structure and alignment of the skull, as well as any abnormal findings that may indicate underlying pathology.
During the examination, the provider assesses the size, shape, and symmetry of the skull. They palpate the bony prominences, such as the frontal and parietal bones, to check for any tenderness or irregularities. They also evaluate the fontanelles in infants, which can give clues about cranial development and hydration status.
- Abnormal findings
Abnormal findings during the assessment of the skull may include craniosynostosis, which is the premature fusion of the cranial sutures. This can lead to abnormal skull shape and potential neurological implications. Other abnormalities that may be detected include bulges or depressions in specific areas of the skull, which may indicate underlying lesions or trauma.
The evaluation of the skull is an integral part of the HEENT exam, allowing healthcare providers to identify any potential abnormalities or concerns. This thorough assessment helps guide further diagnostic investigations and appropriate management plans for patients.
Eyes
The examination of the eyes is a crucial part of the Head, Eyes, Ears, Nose, and Throat (HEENT) exam. It provides valuable information about the patient’s visual acuity, eye movements, and overall eye health. During the examination, the physician evaluates the structures of the eye, including the eyelids, conjunctiva, cornea, iris, and pupils.
One of the first steps in examining the eyes is assessing visual acuity using an eye chart. The patient is asked to read letters or numbers of varying sizes from a distance. This test helps determine if the patient has any refractive errors or vision problems. In addition, the physician checks for any abnormalities in the cornea, such as scars or irregularities.
- Next, the physician examines the pupils. Pupillary reactions are assessed by shining a light into the eye and observing the constriction of the pupil. Unequal pupil size or abnormal responses may indicate neurological or ophthalmic conditions.
- The ophthalmoscope is used to examine the internal structures of the eye. The physician looks through the ophthalmoscope to visualize the retina, optic disc, blood vessels, and macula. This evaluation helps detect any signs of retinal detachment, diabetic retinopathy, or other retinal abnormalities.
- The ophthalmoscope is also used to assess the red reflex, which is a reflection of light off the back of the eye. A normal red reflex indicates a clear pathway for light to reach the retina, while a decreased or absent red reflex may be indicative of cataracts or other opacities.
The HEENT exam also includes an assessment of extraocular movements. The patient is instructed to follow the physician’s finger or a pen as it moves in various directions. This test evaluates the function of the cranial nerves that control eye movements and helps identify any weakness or limitations in eye mobility.
Overall, the examination of the eyes provides valuable information about a patient’s visual function and eye health. It helps detect abnormalities, diagnose conditions, and monitor the effectiveness of treatment. Early detection and intervention are crucial for maintaining good eye health and preventing vision loss.
Assessing visual acuity
Visual acuity is a critical part of a normal HEENT exam and is used to evaluate a person’s ability to see objects clearly. There are different methods to assess visual acuity, but the most common and widely used method is the Snellen chart. The Snellen chart consists of lines of letters or numbers that decrease in size as you move down the chart. The person being tested is asked to read the smallest line they can see clearly from a distance of 20 feet.
During the assessment, it is important to ensure proper lighting and to instruct the person being tested to cover one eye while reading the chart. The person should stand or sit at the appropriate distance and read each line aloud, starting from the top. The visual acuity is recorded as a fraction, with the numerator representing the distance at which the person is standing from the chart and the denominator representing the line they were able to read.
For example, a person with normal visual acuity will be able to read the 20/20 line, meaning they can read at 20 feet what a person with normal vision can read at 20 feet. A person with 20/70 vision can only read at 20 feet what a person with normal vision can read at 70 feet. Visual acuity results can vary from person to person and can be impacted by factors such as age, refractive errors, and ocular diseases or conditions.
Inspecting the External Eye
During a normal heent exam, it is important to thoroughly inspect the external eye to assess for any abnormalities or signs of disease. This involves examining various structures of the eye, including the eyelids, eyelashes, conjunctiva, and sclera.
Eyelids: The examiner should carefully observe the position, symmetry, and movement of the eyelids. Any drooping or asymmetry may indicate a problem with the muscles or nerves that control eyelid movement. The presence of redness, swelling, or lesions on the eyelids should also be noted.
Eyelashes: The condition of the eyelashes should be evaluated, looking for any abnormal hair growth or loss. The presence of crusting, scaling, or discharge around the eyelashes may suggest an infection or other underlying condition.
- Conjunctiva: The conjunctiva is the thin, transparent membrane that covers the whites of the eyes and lines the inside of the eyelids. It should appear clear and pink in a normal exam. Redness, irritation, or the presence of bumps or growths on the conjunctiva may indicate an infection or other eye condition.
- Sclera: The sclera, or the whites of the eyes, should be white in a normal exam. The presence of yellowing (jaundice) or other discoloration may suggest liver or systemic disease. Any visible blood vessels or bulging of the sclera should also be noted, as these may indicate inflammation or other underlying issues.
Overall, a thorough inspection of the external eye is essential in assessing the overall health and potential disorders of the eyes. Any abnormalities found during this examination should be documented and further investigated if necessary.
Ears
During the normal HEENT (head, eyes, ears, nose, and throat) exam, the ears are examined for any abnormalities or signs of infection. The external ear is inspected for any redness, swelling, or discharge. The ear canal is examined using an otoscope, a handheld instrument with a light and magnifying lens. The otoscope allows the healthcare provider to visualize the ear canal and eardrum.
The healthcare provider will assess the eardrum for any signs of perforation, fluid accumulation, or infection. The color and position of the eardrum are noted, as well as the presence of any abnormalities such as scarring or retraction. The mobility of the eardrum is also evaluated by using a pneumatic otoscope, which delivers a small amount of air into the ear canal to assess its response.
If there are any concerns or symptoms suggestive of an ear infection, further tests such as a tympanometry or a hearing test may be recommended. Tympanometry is a non-invasive test that measures the movement of the eardrum in response to changes in air pressure. A hearing test, also known as audiometry, measures the individual’s ability to hear sounds at different frequencies and intensities.
- Inspect external ear for redness, swelling, or discharge
- Examine ear canal using an otoscope
- Assess eardrum for signs of perforation, fluid accumulation, or infection
- Evaluate eardrum mobility using a pneumatic otoscope
- Consider additional tests such as tympanometry or hearing test if necessary